|
|
检索:刘金淑
翻译:赵博
审核:刘金淑、陈志锦
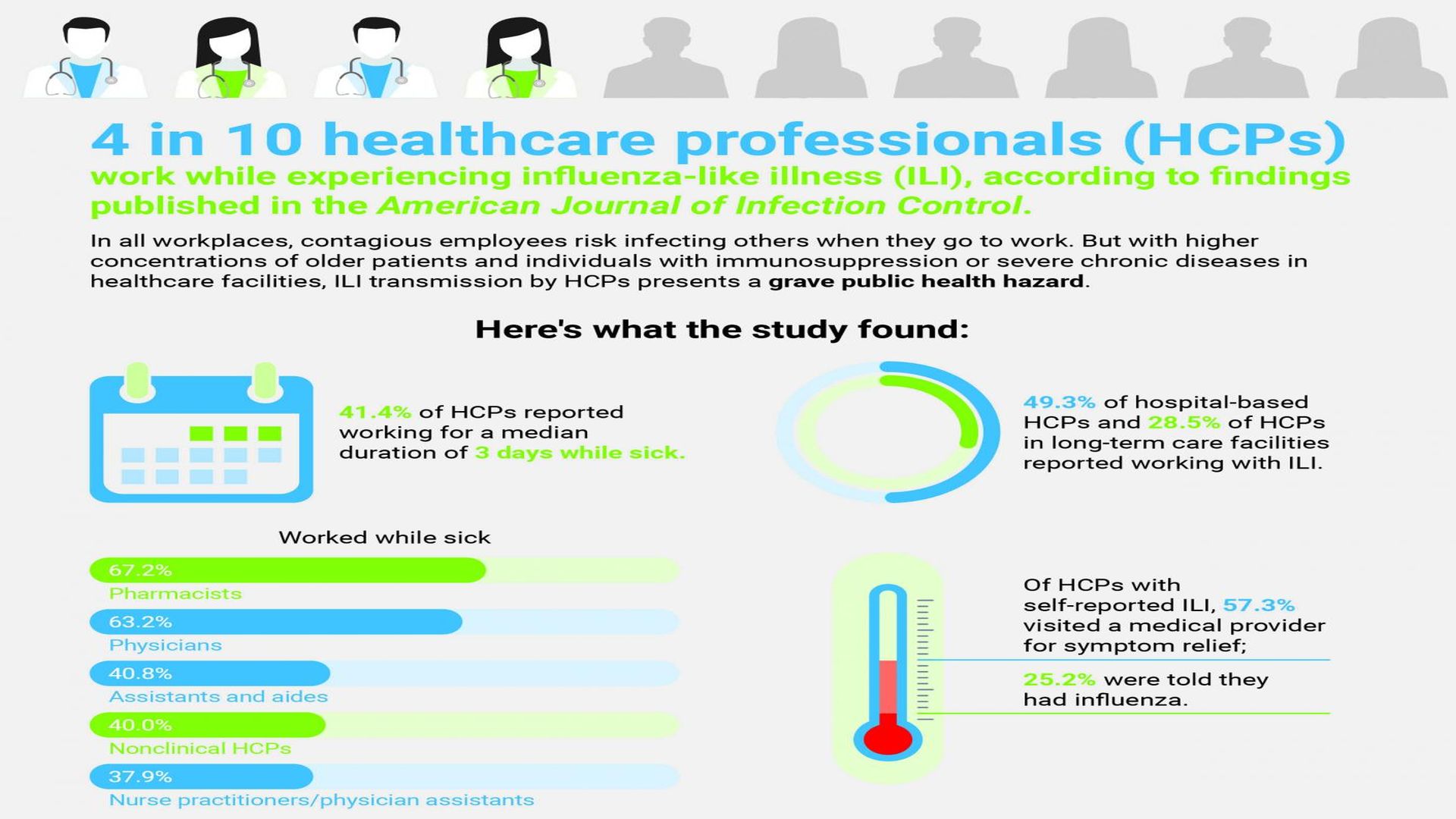
一项新的研究表明,医疗专业人员(HCPs)应该听从他们自己的身体劝告:生病时呆在家里。根据《美国感染控制杂志》(AJIC)11月刊上发表的研究结果,在10位医疗专业人员中,有4位在感染流感样症状的同时仍然工作。与所有工作场所一样,具有传染性的人员上班时可能会存在传染他人的风险。
然而,在医疗机构中,高龄患者和免疫抑制患者或严重慢性疾病患者的比例较高,由专业医护人员传播的流感样疾病会对公共健康造成严重危害。
美国疾控中心国家职业安全与健康研究所首席研究员Sophia Chiu博士表示:“统计数据令人担忧,至少有一项早期的研究表明,接触过患病医疗专业人员的患者,患上相关感染的几率是其他患者的五倍。我们建议所有的医疗机构采取措施支持并鼓励他们的员工在生病期间不要工作”。
通过全国在线调查进行的年度研究收集了2014-2015年流感季节期间1914个医疗专业人员的数据。以受访者自我报告流感样疾病形式,其定义为发烧、合并咳嗽或喉咙痛,并列出促使他们去上班的因素。
该调查评估了多个机构的各种卫生职业:医生、执业护士、助理医师、护士、药剂师、助理/助手、其他临床医疗专业人员、非临床医疗专业人员和学生。评估了四种工作环境:住院部、门诊护理或医生办公室、长期护理机构、其他临床机构。
调查结果:
- 在接受调查的1914名医疗专业人员中,414人报告了流感样疾病。在这些报告中,有183人(占41.4%)在患流感样疾病时的平均持续工作时间为3天。
[/*] - 医院的医疗专业人员工作中与患流感样疾病的接触频率最高,约49.3%,而长期护理设施的医疗专业人员为28.5%,其中临床医疗专业人员为44.3%,药剂师为67.2%、内科医生为63.2%。
[/*] - 相比之下,调查发现约40.8%助理和助手、40.4%非临床医疗专业人员、37.9%护理从业人员/医生助理,32.1%其他临床专业医护人员存在带病工作。
[/*] - 医疗专业人员选择放弃休病假最常见的原因包括:觉得自己仍然可以履行其工作职责;感觉没有“足够糟糕”而呆在家里;认为自己好像没有传染性;感觉自己有义务和同事一起工作;很难找到一个同事来替班。在那些认为自己仍然可以履行工作职责的医疗专业人员中,有39.0%的人因自身流感样症状而寻求医疗服务,54%的人认为自己没有传染性。49.8%的长期护理机构的专业医护人员在生病仍然工作,因为他们不能失去工资。
[/*] - 此前公布的调查结果显示,只有77.3%的受访者表示接受过流感疫苗注射。美国卫生与公众服务部(U.S. Department of Health and Human Services)的“2020年健康人群计划”目标为专业医护人员接种流感疫苗达到90%。
[/*] - 自我报告流感样疾病医疗专业人员的缺席工作天数中位数为2个工作日。在这群人中,57.3%的人为了缓解症状而就医;25.2%的人被告知患有流感。美国疾病预防控制中心(CDC)建议,任何有流感症状的人都要在发烧后等待24小时才能再次工作。
[/*]
从1976年到2007年,在美国与流感相关的死亡人数最高可达16.7/10万人,与流感相关的死亡主要影响到65岁及以上的人。流感在症状发作的前一天至症状出现的七天后均可传播。
来源:APIC
原文
Survey Finds 4 in 10 Healthcare Professionals Work While Sick
A new study suggests that healthcare professionals (HCPs) should heed to their own advice: stay home when sick. Some four in 10 HCPs work while experiencing influenza-like illness (ILI), according to findings published in the November issue of the American Journal of Infection Control (AJIC). As in all workplaces, contagious employees risk infecting others when they turn up for work. But with higher concentrations of older patients and individuals with immunosuppression or severe chronic diseases in healthcare facilities, ILI transmission by HCPs presents a grave public health hazard.
“The statistics are alarming. At least one earlier study has shown that patients who are exposed to a healthcare worker who is sick are five times more likely to get a healthcare-associated infection,” said lead researcher Sophia Chiu, MD, MPH, CDC’s National Institute for Occupational Safety and Health. “We recommend all healthcare facilities take steps to support and encourage their staff to not work while they are sick.”
The annual study, conducted via a national online survey, collected data from 1,914 HCPs during the 2014-2015 influenza season. Respondents self-reported ILI, defined as the combination of a fever and cough or sore throat, and listed factors that prompted them to turn up for work.
The survey assessed a variety of health occupations across multiple institutions: physicians; nurse practitioners and physician assistants; nurses; pharmacists; assistants/aides; other clinical HCP; nonclinical HCPs; and students. Four types of work settings were assessed: hospitals; ambulatory care or physician offices; long-term care facilities; or other clinical settings.
Among the findings:
• Of the 1,914 HCPs surveyed, 414 reported ILI. Of these, 183—or 41.4 percent—reported working for a median duration of three days while experiencing influenza-like symptoms.
• Hospital-based HCPs had the highest frequency of working with ILI (49.3 percent), compared to HCPs at long-term care facilities (28.5 percent). Clinical professional HCPs were the most likely to work with ILI (44.3 percent), with pharmacists (67.2 percent) and physicians (63.2 percent) among those with the highest frequency.
• In contrast, the survey found that assistants and aides (40.8 percent), nonclinical HCPs (40.4 percent), nurse practitioners/physician assistants (37.9 percent), and other clinical HCPs (32.1 percent) worked while sick.
• The most common reasons for HCPs to opt from taking sick leave included feeling that s/he could still preform his/her job duties; not feeling “bad enough” to stay home; feeling as if s/he were not contagious; sensing a professional obligation to be present for coworkers; and difficulty finding a coworker to cover for him/her. Among the HCPs who felt they could still preform their job duties, 39.0 percent sought medical attention for their ILI symptoms, as did 54.0 percent of those who did not think they were contagious. 49.8 percent of HCPs in long-term care settings who reported for work when sick reported doing so because they couldn’t afford to lose the pay.
• Previously published results from this survey described that only 77.3 percent of respondents reported receiving a flu shot. The U.S. Department of Health and Human Services’ Healthy People 2020 aims to reach a 90 percent influenza vaccination rate for HCPs.
• HCPs with self-reported ILI missed a median number of two work days. Of this cohort, 57.3 percent visited a medical provider for symptom relief; 25.2 percent were told they had influenza. The Centers for Disease Control and Prevention recommends that anyone with ILI wait 24-hours after a fever breaks before returning to work.
“Patients’ health and wellbeing are at stake when contagious HCPs opt not to stay home. Tailored strategies per occupation and health institution, including updating paid sick leave policies, can empower HCPs to make healthy choices not only for themselves, but for their coworkers and patients,” said Linda Greene, RN, MPS, CIC, FAPIC, 2017 APIC president.
From 1976-2007, influenza-associated fatalities accounted for up to 16.7 (ranged between 1.4 and 16.7) deaths per 100,000 people in the U.S. Flu-related deaths predominantly impact individuals 65 years and older. Influenza may be transmissible from one day before, and up to seven days after, symptoms onset.
Vis Reference: “Working with influenza-like illness: Presenteeism among US health care personnel during the 2014-2015 influenza season,” by Sophia Chiu, MD, MPH; Carla L. Black, PhD; Xin Yue, MPS, MS; Stacie M. Greby, DVM, MPH; A. Scott Laney, PhD; Angela P. Campbell, MD, MPH; and Marie A. de Perio, MD, appears in the American Journal of Infection Control, Volume 45, Issue 11 (November 2017).
Source: APIC
图文编辑:小小牧童
|
|